🚀 Catch Marvix at the 2026 Annual Meeting of the Florida Society of Neurology (FSN) | Jan 17–18 | Orlando, FL | Booth #24 🎉

Twenty-two minutes.
That's how long it takes to review a returning patient's chart before a fifteen-minute consult for specialities like oncology, neurology etc.
Not because you're slow. Because her clinical story is buried in three EHR systems, two imaging centers, faxed lab reports, scanned consult letters, and a handwritten intake form from last month.
The information exists. It just doesn't exist together.
What if it could exist together and all of that could happen automatically? Could it be possible?
Yes, it is. Enter Marvix AI Summarizer - our latest feature, built to unify the past and the present (and also the only AI assistant offering this in a trial ;) ).
It ingests clinical information across any format, any source and structures it as a cohesive summary, while ensuring that no piece of relevant history gets left behind. And you can go into every consultation with complete context.
Quite simply, the AI Summarizer does two things:
1. It generates a Patient Recap. A unified summary of everything clinically relevant from the patient's history, organized by category and time.
2. It inserts historical context directly into the current visit note. As you document today's consult, Marvix adds relevant information from prior diagnoses, treatments, labs, and imaging into the relevant sections.
The result is a note that connects past and present information without manual copy-pasting or toggling between systems.
Literally everything (document related ;))!
Marvix processes clinical information from any source, available in any format. Data flows through automated retrieval from integrated EHR systems or through manual uploads.
In short - If it exists in the chart, Marvix can read it, structure it, and summarize it!
Here are some of the clinical documents that Marvix AI Summarizer can ingest:
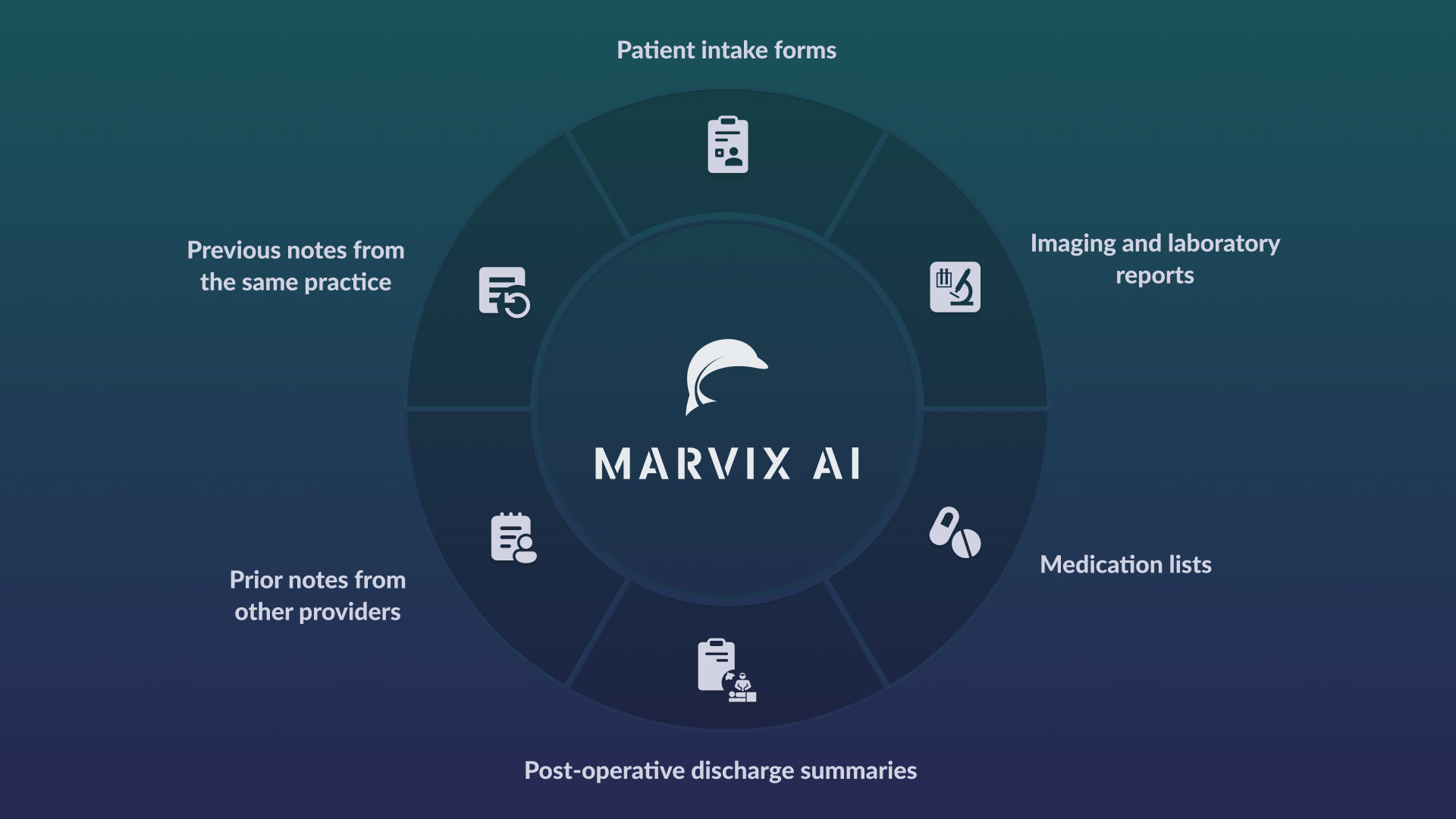
And here’s a list of sources and formats that Marvix AI summarizer can process from:
.png)
Once all available data is provided and processed by our AI Summarizer, Marvix generates the Patient Recap in a couple of minutes. And you get a structured summary, capturing all key points and information from the data/ documents shared, that can be reviewed before the consult begins.
Here’s what a patient recap gives you
The recap organizes clinical information by category and time:
Each recap includes a chronological timeline and an interval summary that highlights what changed between visits.
The recap can be configured to match the provider’s workflow. Marvix can adjust the level of detail, section order, and terminology style based on the specialty and documentation preferences.
Here’s a real life example of how Marvix AI summarizer works:
Let's take a case of a patient diagnosed with cancer for over 4 years and is meeting an oncologist who is using Marvix AI.
Emily Carter is a breast cancer survivor treated with endocrine therapy. Over the past months, she has experienced worsening fatigue, persistent morning joint stiffness, and intermittent left arm swelling. Previous labs and imaging have shown no evidence of cancer recurrence. Her prior history also includes osteopenia and early signs of lymphedema noted on earlier follow-ups.
The oncologist wants a comprehensive and efficient understanding of the case. His connected EHR pulls previous notes, lab reports, and imaging from the past 4 years. He also manually uploads some handwritten notes from her last few visits.
Marvix ingests Emily's whole clinical journey and generates a longitudinal summary of her case from the first visit. Here’s a view of the output generated by the AI summarizer:
1. Summary of previous notes:
.png)
This image displays the Patient Recap summary view of prior clinical notes generated by the AI Summarizer. The section includes a structured history of present illness with diagnosis details, surgical history, treatment initiation dates, symptom progression, and relevant past medical history. Information from multiple prior visits is organized into clear sections.
.png)
This image shows the Patient Recap summary that includes labs, imaging, assessment, plan, and diagnoses. Historical findings such as prior imaging results, lab timelines, and ongoing conditions are are organised into neat sections.
.png)
This image displays the Patient Recap summary view of laboratory and imaging data collected over multiple years. The section includes bone density measurements with dates, laboratory values such as vitamin D levels, and a list of relevant trends over time. Results are grouped by category and presented in chronological order.
Marvix AI ingests years of notes, labs, and imaging from multiple sources and formats, organizes them into a longitudinal clinical summary, reducing chart review time and helping clinicians start each visit with complete context.
Marvix goes one step ahead of the Patient Recap to generate Composite Notes. These notes merge the context of prior history with data captured during the current visit.
In a standard clinical note, historical data lives in discrete sections such as past history or prior results. This information exists in the chart but often remains separate from the current assessment and plan.
In a Composite Note, historical information is referenced directly within the present visit note. Assessments reflect prior findings. Plans account for prior therapies, timelines, and interval results. The note presents past and present information within the same narrative structure.
The system aligns historical information with new observations, creating a single note that reflects both longitudinal continuity and the present encounter.
Key Components of Composite Notes
The result is a note that connects what happened before with what happened today.
Here’s a real life example of what a Composite note looks like:
Let's take the same case as earlier, of Emily Carter, a patient diagnosed with cancer for over 4 years and is meeting an oncologist who is using Marvix AI.
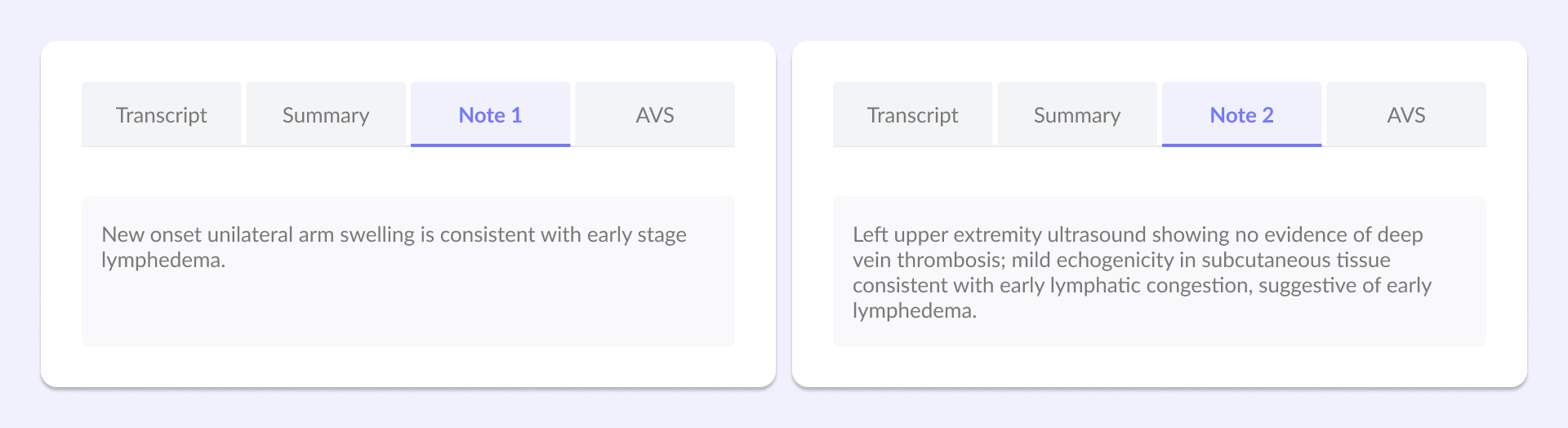
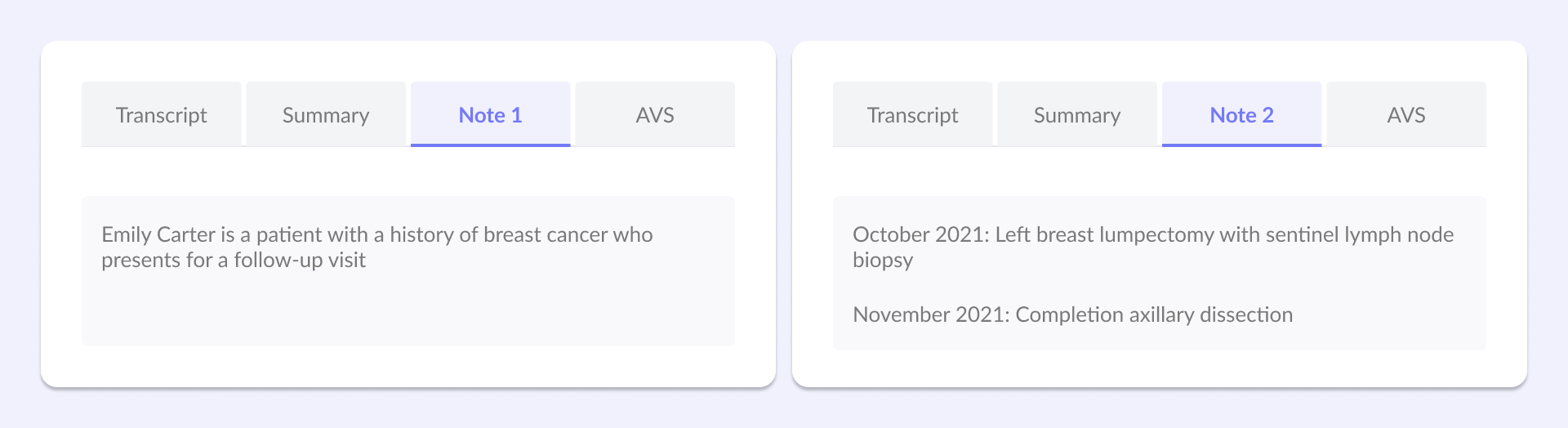
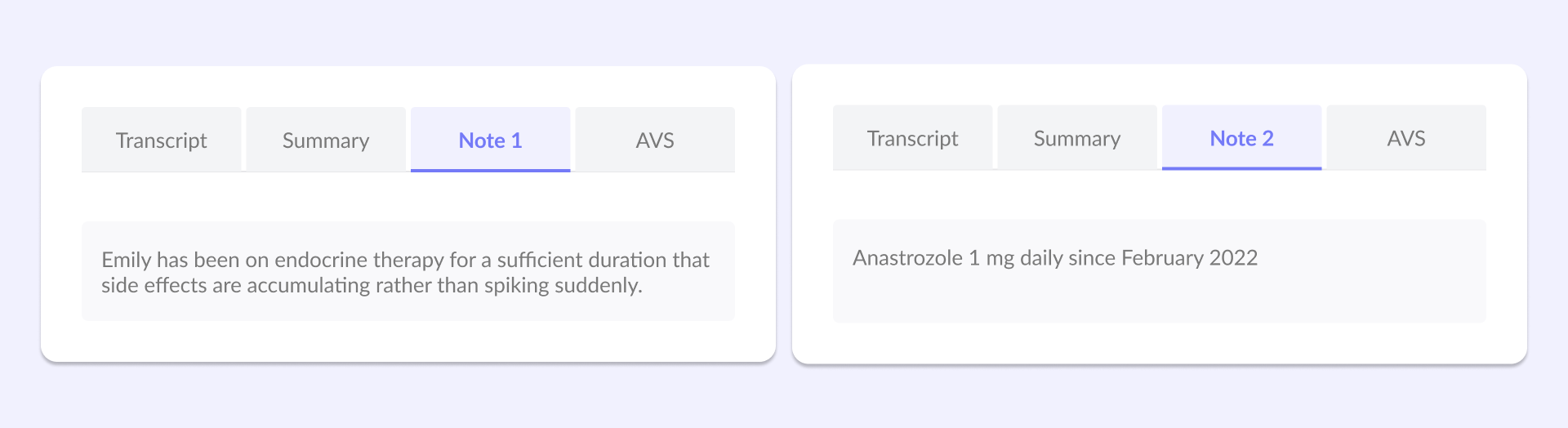
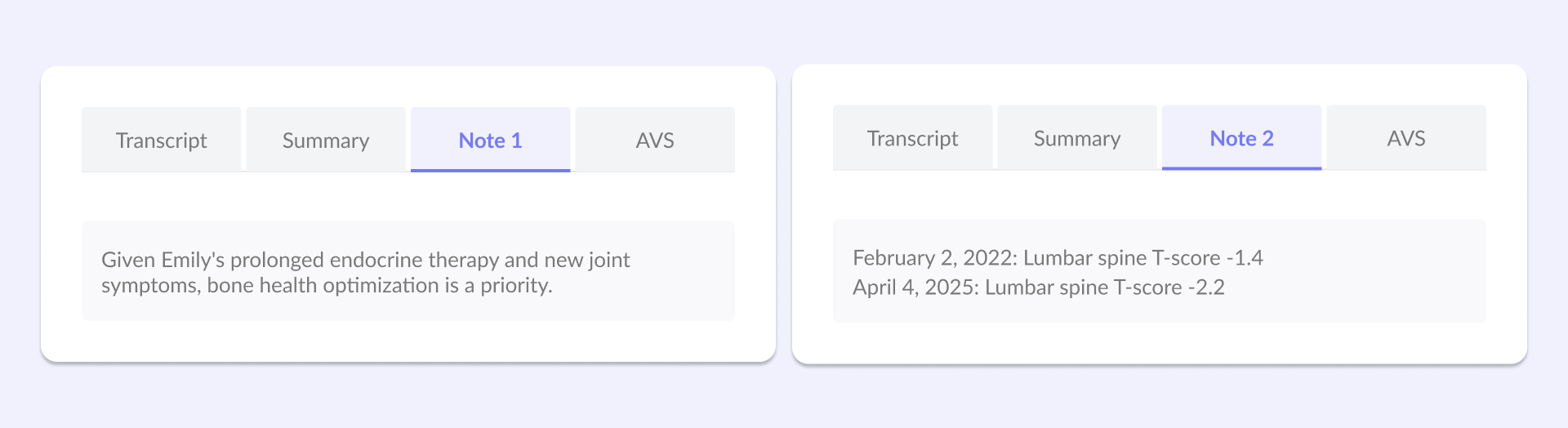
To illustrate how this feature works in practice, two clinical notes have been generated for Emily's current visit using Marvix:
Note 1: Current visit only. This note documents today's consultation without any historical context. It captures what Emily reports and what the oncologist observes during this visit alone.
Note 2: Current visit + AI Summarizer. This note includes everything from Note 1, but Marvix has processed 4 years of historical data and woven relevant context throughout. Past diagnoses, treatment responses, lab trends, and imaging findings are integrated into the appropriate sections.
Here's the difference:
1. Lymphedema Evaluation Beyond Symptom Description
2. Surgical context
3. Endocrine therapy timeline
4. Bone health trajectory
This contrast shows how prior findings shift from being implied or absent to being clearly documented within the Composite note, when historical documents were present.
For example, for Lymphedema Evaluation, Note 1 reflects the current clinical impression while Note 2 incorporates prior diagnostic evaluation as shown blow:
Note 1: “New onset unilateral arm swelling is consistent with early stage lymphedema.”
Note 2: “Left upper extremity ultrasound showing no evidence of deep vein thrombosis; mild echogenicity in subcutaneous tissue consistent with early lymphatic congestion, suggestive of early lymphedema.”
Marvix AI reads years of fragmented clinical history and weaves relevant diagnoses, procedures, timelines, and test results directly into the current visit note, making a Composite Note, ensuring prior context is present wherever relevant.
That’s how 22 minutes of chart review becomes just 2.
With Marvix’s AI summariser, the heavy lifting is already done before the visit begins. The chart has been reviewed, the longitudinal timeline reconstructed, and the relevant historical context surfaced directly in the Patient Recap. Fragmented records across EHRs, scanned documents, and prior notes are unified into structured summaries, with key diagnoses, timelines, and prior treatments automatically embedded into today’s note.
So when the patient walks in, you’re no longer piecing together history—you’re already oriented, informed, and ready to focus on a well-reasoned assessment and plan.
And yes, the information finally exists in one place.
What once felt impractical, if not impossible, is now available in routine clinical practice. If you’re curious to see how this fits into your workflow, we’re happy to set it up for you. Book a demo and explore a 30-day free trial - no commitments, just full access to Marvix’s capabilities, including the AI summarizer.